Hey everyone, do you suffer Staphylococcus aureus?, we’ve got you 10 best treatments of Staphylococcus aureus with herbs, these herbs are proven to be curative agents to Staphylococcus aureus, do well to read through and be enriched.
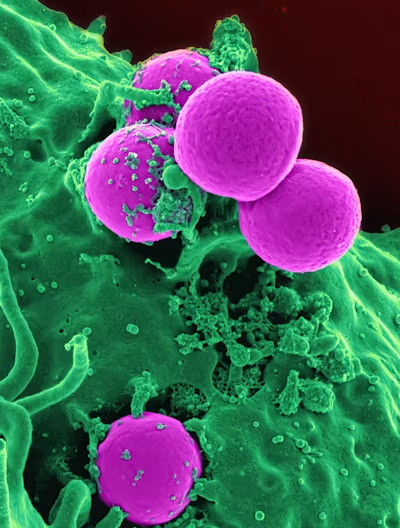
Staphylococcus aureus is a bacterium commonly found on the skin and in the respiratory tract of humans. It is a Gram-positive, round-shaped bacterium that forms clusters resembling grapes when viewed under a microscope.
While S. aureus is typically harmless and may even be part of the normal flora of the human body, it can also cause a wide range of infections if it enters the body through cuts, wounds, or other openings. These infections can vary from minor skin infections like boils and pimples to more serious conditions such as pneumonia, meningitis, and bloodstream infections.
One of the concerning aspects of S. aureus is its ability to develop resistance to antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of S. aureus that has become resistant to many antibiotics, making it difficult to treat and posing a significant public health challenge.
- aureus can produce a variety of toxins and enzymes that contribute to its pathogenicity, allowing it to evade the immune system and cause tissue damage. It can also form biofilms, which are communities of bacteria encased in a protective matrix, making them even more resistant to antibiotics and immune responses.
Preventing S. aureus infections often involves good hygiene practices such as regular handwashing, proper wound care, and avoiding contact with contaminated surfaces. In healthcare settings, infection control measures such as strict hand hygiene, isolation precautions, and appropriate use of antibiotics are crucial for preventing the spread of S. aureus infections, particularly those caused by MRSA.
Characteristics of Staphylococcus aureus, 10 best treatments of Staphylococcus aureus with herbs
Gram-Positive: Staphylococcus aureus is a gram-positive bacterium, meaning it retains the purple color of the primary stain in the Gram stain technique.
Spherical Shape: It typically appears as spherical (cocci) bacteria under the microscope.
Clustered Arrangement: Staphylococcus aureus often forms clusters resembling bunches of grapes when viewed under the microscope, hence its name “staphylo” (clusters).
Golden Pigment: When cultured on agar plates, some strains of Staphylococcus aureus produce a characteristic golden or yellow pigment, giving rise to its name “aureus” (golden).
Facultative Anaerobe: Staphylococcus aureus can grow in both the presence and absence of oxygen.
Catalase-Positive: It produces the enzyme catalase, which allows it to convert hydrogen peroxide into water and oxygen, producing bubbles when hydrogen peroxide is added to a colony of Staphylococcus aureus.
Non-Motile: Staphylococcus aureus is generally non-motile and does not possess flagella for movement.
Salt-Tolerant: It can grow in high salt concentrations, which is why it is commonly found on the skin and mucous membranes where salt (sweat) is present.
Beta-Hemolytic: Some strains of Staphylococcus aureus produce beta-hemolysin, an exotoxin that causes complete lysis of red blood cells, leading to a clear zone around bacterial colonies on blood agar plates.
Coagulase-Positive: Staphylococcus aureus produces the enzyme coagulase, which causes the conversion of fibrinogen to fibrin, leading to the formation of clots.
Capsule Formation: It has the ability to form a polysaccharide capsule, which aids in evasion of the host immune response.
Biofilm Formation: Staphylococcus aureus can produce biofilms, which are complex communities of bacteria embedded in a self-produced extracellular matrix. Biofilms enhance bacterial survival and resistance to antibiotics.
Toxin Production: Staphylococcus aureus produces a variety of toxins, including enterotoxins, exfoliative toxins, and toxic shock syndrome toxin-1 (TSST-1), which contribute to its pathogenicity.
Antibiotic Resistance: Staphylococcus aureus has the ability to develop resistance to multiple antibiotics, including methicillin, making treatment challenging in some cases.
Pathogenicity Islands: Staphylococcus aureus possesses pathogenicity islands, which are clusters of genes encoding virulence factors that contribute to its ability to cause disease.
These characteristics collectively contribute to the pathogenicity and resilience of Staphylococcus aureus, making it a significant human pathogen with a wide range of clinical manifestations.
The Many Faces of Staphylococcus aureus
indeed, Staphylococcus aureus is a highly versatile bacterium with a knack for causing a diverse array of infections. Its adaptability and resilience stem from a combination of factors, including its ability to produce various virulence factors, its capacity to form biofilms, and its propensity for acquiring antibiotic resistance.
Here’s a glimpse into the many faces of Staphylococcus aureus infections:
Skin and Soft Tissue Infections (SSTIs): S. aureus is a common culprit behind a range of skin infections, from minor ones like folliculitis and impetigo to more severe conditions such as cellulitis, abscesses, and wound infections. These infections can be localized or spread more extensively, posing risks of systemic complications.
Surgical Site Infections (SSIs): Following surgical procedures, S. aureus can infiltrate incision sites, leading to SSIs. These infections can prolong hospital stays, delay wound healing, and increase the risk of more serious complications, particularly if the bacterium gains access to deeper tissues or organs.
Pneumonia: S. aureus is a common cause of both community-acquired and healthcare-associated pneumonia. In vulnerable populations, such as the elderly, infants, and immunocompromised individuals, S. aureus pneumonia can be severe and life-threatening.
Bloodstream Infections (Bacteremia): When S. aureus enters the bloodstream, it can cause bacteremia, which can lead to sepsis, a potentially deadly systemic inflammatory response. Bloodstream infections with S. aureus are particularly concerning due to the bacterium’s ability to spread rapidly to vital organs.
Bone and Joint Infections: S. aureus can also invade bones and joints, causing osteomyelitis (bone infection) or septic arthritis. These infections are challenging to treat due to poor antibiotic penetration into bone tissue and the formation of biofilms on prosthetic joints.
Toxic Shock Syndrome (TSS): Certain strains of S. aureus produce toxins, such as toxic shock syndrome toxin-1 (TSST-1), which can lead to TSS—a rare but severe illness characterized by high fever, rash, low blood pressure, and multiple organ failure.
Endocarditis: Infections of the heart valves (endocarditis) can occur when S. aureus enters the bloodstream and colonizes the heart valves. Endocarditis can damage heart tissue and cause life-threatening complications if not promptly treated with antibiotics and, in some cases, surgical intervention.
Device-Associated Infections: S. aureus readily forms biofilms on medical devices like central venous catheters, urinary catheters, and prosthetic implants. These biofilms provide a protective environment for the bacteria, making infections difficult to eradicate and increasing the risk of treatment failure.
Given its versatility and the challenges it poses in both community and healthcare settings, combating Staphylococcus aureus infections requires a multifaceted approach, including infection control measures, judicious antibiotic use, and ongoing research into new treatment strategies.
Challenges of Antibiotic Resistance
Antibiotic resistance is a significant challenge in the management of Staphylococcus aureus infections, particularly with the emergence and spread of methicillin-resistant Staphylococcus aureus (MRSA) strains. Here are some key challenges associated with antibiotic resistance in S. aureus:
Limited Treatment Options: MRSA strains are resistant to beta-lactam antibiotics, such as methicillin, penicillin, and cephalosporins, which are commonly used to treat bacterial infections. This resistance narrows the range of effective antibiotics, limiting treatment options and increasing the risk of treatment failure.
Increased Morbidity and Mortality: Infections caused by antibiotic-resistant S. aureus are associated with higher rates of treatment failure, complications, and mortality compared to infections caused by susceptible strains. Patients with MRSA infections often require more prolonged hospitalizations, intensive care, and costly treatments.
Cross-Resistance: MRSA strains often exhibit resistance to multiple classes of antibiotics, including not only beta-lactams but also other important antibiotics like fluoroquinolones, macrolides, and aminoglycosides. This cross-resistance further limits the available therapeutic options and complicates treatment decisions.
Spread in Healthcare Settings: MRSA can spread readily in healthcare facilities, leading to outbreaks and endemic transmission. Patients in hospitals and long-term care facilities are particularly vulnerable to MRSA infections due to factors such as frequent antibiotic use, invasive procedures, and close proximity to other patients with infections.
Community-Acquired Infections: While MRSA was historically associated with healthcare settings, community-acquired MRSA (CA-MRSA) strains have emerged and become a significant public health concern. CA-MRSA strains often cause skin and soft tissue infections in otherwise healthy individuals and can spread rapidly within households, schools, and other community settings.
Challenges in Eradication: MRSA can persist in the environment and colonize the skin and mucous membranes of individuals, serving as a reservoir for transmission. Eradicating MRSA from healthcare facilities and communities is challenging due to its ability to survive on surfaces and its potential for asymptomatic carriage.
Development of Resistance Mechanisms: S. aureus has a remarkable ability to acquire and exchange genetic elements, including resistance determinants, through horizontal gene transfer. This genetic plasticity allows S. aureus to rapidly develop new mechanisms of antibiotic resistance, further complicating treatment efforts.
Addressing the challenge of antibiotic resistance in Staphylococcus aureus requires a multifaceted approach, including prudent antibiotic use, infection prevention and control measures, development of new antibiotics, and investment in alternative therapies such as bacteriophage therapy and immunotherapies. Additionally, promoting antimicrobial stewardship programs and public awareness campaigns can help mitigate the spread of resistant strains and preserve the effectiveness of existing antibiotics.
Staphylococcus aureus infections
Staphylococcus aureus infections are caused by the bacterium Staphylococcus aureus, commonly referred to as “staph.” This bacterium is often found on the skin or in the nasal passages of healthy individuals and does not usually cause any harm. However, if it enters the body through a cut, wound, or other opening, it can cause infections ranging from minor skin infections to more serious conditions such as pneumonia, bloodstream infections, or toxic shock syndrome.
Here are some key points about Staphylococcus aureus infections:
- Skin Infections: Staphylococcus aureus is a common cause of skin infections, including boils, impetigo, cellulitis, and folliculitis. These infections typically present as red, swollen, and painful areas on the skin.
- Wound Infections: Staphylococcus aureus can infect wounds, particularly if they are not properly cleaned and dressed. This can lead to complications such as abscess formation or delayed wound healing.
- Soft Tissue Infections: In addition to skin and wound infections, Staphylococcus aureus can cause infections in deeper tissues, such as muscles or fascia, leading to conditions like myositis or necrotizing fasciitis.
- Systemic Infections: In severe cases, Staphylococcus aureus can enter the bloodstream and cause systemic infections such as bacteremia or sepsis. These infections can be life-threatening if not promptly treated with appropriate antibiotics.
- Resistant Strains: Staphylococcus aureus is notorious for developing resistance to antibiotics. Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of the bacterium that is resistant to multiple antibiotics, making it more difficult to treat.
Treatment of Staphylococcus aureus infections typically involves antibiotics, although the choice of antibiotic may depend on the strain’s susceptibility to different drugs. In additio n to antibiotics, proper wound care and hygiene practices are essential for preventing and controlling Staphylococcus aureus infections.
10 best treatments of Staphylococcus aureus with herbs
While herbs are often explored for their potential medicinal properties, it’s important to note that Staphylococcus aureus infections can be serious and may require medical treatment, including antibiotics prescribed by a healthcare professional. However, some herbs have been studied for their antimicrobial properties and may offer complementary support in managing infections. Here are ten herbs that have shown promise in laboratory studies for their antibacterial effects against Staphylococcus aureus:
Garlic (Allium sativum): Garlic contains allicin, a compound known for its antimicrobial properties. Some studies suggest that garlic extract may inhibit the growth of Staphylococcus aureus.
Turmeric (Curcuma longa): Curcumin, the active compound in turmeric, has demonstrated antibacterial activity against Staphylococcus aureus in laboratory studies.
Oregano (Origanum vulgare): Oregano contains carvacrol and thymol, compounds with antimicrobial properties. Oregano oil has been shown to inhibit the growth of Staphylococcus aureus in vitro.
Tea Tree (Melaleuca alternifolia): Tea tree oil has strong antimicrobial properties and has been investigated for its effectiveness against Staphylococcus aureus in topical applications.
Echinacea (Echinacea purpurea): Echinacea is traditionally used to support the immune system. Some research suggests that compounds in echinacea may have antimicrobial effects against Staphylococcus aureus.
Goldenseal (Hydrastis canadensis): Berberine, a compound found in goldenseal, has demonstrated antibacterial activity against Staphylococcus aureus in laboratory studies.
Manuka Honey: Manuka honey has potent antimicrobial properties due to its high levels of methylglyoxal. It has been investigated for its ability to inhibit the growth of Staphylococcus aureus and promote wound healing.
Thyme (Thymus vulgaris): Thyme contains thymol and carvacrol, which have been shown to have antimicrobial effects against Staphylococcus aureus.
Cinnamon (Cinnamomum verum): Cinnamon contains cinnamaldehyde, which has demonstrated antibacterial activity against Staphylococcus aureus in laboratory studies.
Ginger (Zingiber officinale): Ginger contains gingerol, which has been investigated for its antimicrobial properties. While research specifically on Staphylococcus aureus is limited, ginger may have potential as a complementary treatment.
It’s essential to remember that while these herbs show promise in laboratory studies, their effectiveness in treating Staphylococcus aureus infections in humans has not been conclusively proven. Additionally, herbal remedies should not be used as a substitute for medical treatment prescribed by a healthcare professional. If you suspect a Staphylococcus aureus infection, it’s crucial to seek medical advice promptly.
Medical treatments of Staphylococcus aureus infections
Antibiotics: Depending on the severity and type of infection, antibiotics are typically the first-line treatment for Staphylococcus aureus infections. Commonly used antibiotics include:
Beta-lactam antibiotics (e.g., penicillin, oxacillin, nafcillin)
Vancomycin
Clindamycin
Linezolid
Daptomycin
Trimethoprim-sulfamethoxazole
Drainage of Abscesses: For skin and soft tissue infections such as abscesses, drainage is often necessary to remove pus and infected material.
Wound Care: Proper wound care is essential for preventing and treating Staphylococcus aureus infections. This may include cleaning the affected area, applying antibiotic ointments, and dressing the wound.
Intravenous Immunoglobulin (IVIG): In some severe cases, IVIG may be used as adjunctive therapy to boost the immune response against Staphylococcus aureus infections.
Surgical Debridement: For deep-seated or necrotizing infections, surgical debridement may be required to remove infected tissue and prevent the spread of the infection.
Antiseptic Washes: Antiseptic solutions such as chlorhexidine or povidone-iodine may be used to cleanse the skin or surgical sites before procedures to reduce the risk of infection.
Intravenous Fluids: Patients with severe infections may require intravenous fluids to maintain hydration and support vital functions.
Pain Management: Pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to alleviate discomfort associated with Staphylococcus aureus infections.
Topical Antibiotics: For localized skin infections, topical antibiotics such as mupirocin may be prescribed to apply directly to the affected area.
Antibiotic Stewardship: In cases of antibiotic-resistant Staphylococcus aureus infections, antibiotic stewardship programs are crucial to ensure appropriate antibiotic use and prevent further development of resistance.
Isolation Precautions: In healthcare settings, patients with Staphylococcus aureus infections may be placed on contact precautions to prevent the spread of the bacteria to others.
Probiotics: Some studies suggest that probiotics may help restore the balance of gut flora and reduce the risk of Staphylococcus aureus colonization or infection, particularly in vulnerable populations.
Immune Modulators: In certain cases, immune modulating medications such as corticosteroids or immunomodulatory agents may be used to modulate the immune response to Staphylococcus aureus infections.
Intravenous Antibiotic Therapy: Severe infections may require intravenous administration of antibiotics for more effective delivery and rapid control of the infection.
Antibiotic Combination Therapy: In cases of complicated or resistant infections, combination therapy with two or more antibiotics may be used to improve efficacy and prevent the development of resistance.
It’s important to note that treatment decisions should be made in consultation with a healthcare professional based on the specific circumstances and characteristics of the infection. Prompt and appropriate treatment is crucial for preventing complications and promoting recovery from Staphylococcus aureus infections.
Conclusion
While herbs can have antimicrobial properties, treating Staphylococcus aureus solely with herbal remedies may not be sufficient, especially in severe cases. However, incorporating herbs into a comprehensive treatment plan alongside conventional antibiotics and medical care may offer additional benefits. Here are ten herbs that have shown potential in combating Staphylococcus aureus:
Garlic: Known for its antimicrobial properties, garlic contains allicin, a compound with potent antibacterial effects.
Turmeric: Curcumin, the active compound in turmeric, exhibits antimicrobial activity against various pathogens, including Staphylococcus aureus.
Ginger: Gingerol and other compounds in ginger possess antibacterial properties that may help combat Staphylococcus aureus.
Oregano: Rich in carvacrol and thymol, oregano oil has demonstrated antimicrobial activity against Staphylococcus aureus.
Thyme: Thyme contains thymol, carvacrol, and other compounds with antimicrobial properties that may inhibit the growth of Staphylococcus aureus.
Echinacea: This herb is known for its immune-boosting properties and may help support the body’s natural defenses against Staphylococcus aureus infections.
Tea Tree Oil: Tea tree oil has powerful antimicrobial properties and may be effective against Staphylococcus aureus when applied topically.
Goldenseal: Berberine, a compound found in goldenseal, exhibits antimicrobial activity and may help combat Staphylococcus aureus infections.
Manuka Honey: With its high concentration of methylglyoxal, Manuka honey has potent antibacterial properties and may aid in wound healing, including those caused by Staphylococcus aureus infections.
Cinnamon: Cinnamon contains cinnamaldehyde, which has antimicrobial properties and may help inhibit the growth of Staphylococcus aureus.
While these herbs show promise, it’s crucial to consult with a healthcare professional before using them, especially if you have a severe infection. Additionally, herbal remedies should complement, not replace, conventional medical treatment for Staphylococcus aureus infections.